A 35 YEAR OLD MALE WITH C/O SOB
This is an E log book to discuss our patient's de-identified health data shared after taking his guardian's signed informed consent. Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable comments in comment box are most welcomed
I have been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency i reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CASE DISCUSSION:
A 35 year old male came with complaints of
- fever since 5 days
- cough since 2 days
- breathlessness since 1 day
HOPI:
Pt was apparently assymptomatic 5 days back then developed fever which was high grade,intermittent, and associated with chills, relieved on taking medication not associated with vomitings, burning micturition, loose stools.2 days later patient complained of cough with bloody expectoration and shortness of breath (grade II),aggrevated on lying down and relieved in sitting position.For which he was admitted to a private hospital 1 day back and as the symptoms aggravated he was shifted to our hospital. Presently patient complaints of SOB (grade IV) and cough.
PAST HISTORY: Not a k/c/o DM,htn,tb,asthma,epilepsy
PERSONAL HISTORY:
He is married
Daily wage labourer by occupation (not going to work since 1 month)
Consumes mixed diet
Appetite reduced
Bowel n bladder regular
Sleep adequate
Addictions:
Consumes Alcohol since 15 years, stopped 5 years back on his own will and then started 2 months back, consumes 2 bottles/day (country liquor)
Last consumed 6 days back 1 quater
Consumes khaini (chewable tobacco) since 15 years everyday 2 packs
FAMILY HISTORY:
No similar complaints in family
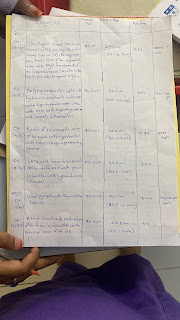
CLINICAL IMAGES:
GENERAL EXAMINATION:
Pt is conscious, coherent and cooperative
Moderately built and nourished.
On admission:
BP:140/80mmhg
PR:66bpm
RR:46cpm
SPO2: 67% on RA
GRBS: 94mg/dl
SYSTEMIC EXAMINATION:
CVS: S1,S2, +
RS: B/L diffuse crepts, air entry decreased in right lower lobe
P/A:Soft, Non tender
CNS: NAD
PROVISIONAL DIAGNOSIS:
COMMUNITY ACQUIRED PNEUMONIA WITH PULMONARY OEDEMA ?ARDS.































Comments
Post a Comment