Period of posting - 11th of August to 11th of October
11/8-26/8
PSYCHIATRY DUTY:
Learned about importance of history taking and how by history we can reach to a provisional diagnosis.
Saw different patients and learned how to take basic history
Examples like :
1. Schizophrenia
2.OCD
3.ALCOHOL DEPENDENCE SYNDROME
4. TOBBACO DEPENDENCE SYNDROME
5. BPAD under remission
Went for DAC saw how pgs interact with the patients
27/8-26/9
UNIT DUTY
Case 1:
https://ailanibyogita.blogspot.com/2022/08/icu-bed-2.html
Patient came to casuality and after all basic investigations was shifted to our Intensive critical care unit.
1) What was the cause of his seizure ?
A: Lesion in the left side of brain
2) What is the further plan of treatment ?
3) As patient had no previous history of seizures and no co-morbidities what could be the reason of sudden presentation?
Unfortunately pt LEFT AGAINST MEDICAL ADVICE (LAMA) for personal reasons.
Case 2:
https://ailanibyogita.blogspot.com/2022/08/22-years-old-male-with-dengue-fever.html
1) Type of rash patient presented with?
Ans: white islands in a sea of red (maculopapular rash)
2) Procedures done:
took iv samples for the patient (lab investigations)
Connected iv fluids to patient
3) patient was discharged after 4 days as symptoms subsided and RAPID DENGUE was negetive
Case 3:
https://ailanibyogita.blogspot.com/2022/09/a-35-years-old-female-with-co-fever.html
1) What was the etiology of her abdominal pain?
Ans: Planned for USG Abdomen: in findings we got evidences of serocites which could probably be due to dengue or viral pyrexia.
As the patient presented with complaints of fever we got
RAPID DENGUE
WIDAL TEST
MALARIA STRIP TEST
done and all turned out be negetive.
As to rule out any infection we even got blood and urine cultures which also presented with no growth.
As pt was having evening rise of temp associated with cough and cold we could be suggesting viral pyrexia.
2) Patient even complained of joint pains (small joints) since 6 months associated with morning stiffness but RA factor came to be non-reactive, what could be other cause ?
Ans: RA factor is not a sensitive factor for RHEUMATOID ARTHRITIS so it can be negetive.
Link for efficacy of RA factor in diagnosis of RA: https://pubmed.ncbi.nlm.nih.gov/1456851/
Others tests done for RA and their sensitivity and specificity: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2695367/
3) Procedures done:
took iv samples and cultures for the patient (lab investigations)
Connected iv fluids to patient
4) patient was discharged after 6 days as symptoms subsided and was advised good healthy diet and multivitamin tablet for her weakness.
Case 4:
1) Patient was presented to us with fever and altered sensorium on the 5th day of fever. What could be the cause of altered sensorium?
Ans: Firstly we tried ruling out all possible organic causes and psychological causes.
Organic causes were ruled out by doing lab investigations.
Psychological causes because pt has a history of alcohol and tobacco consumption since 50 yrs and suffered from recent trauma 2 months back when his wife passed away.
(For the above we had requested for psychiatry referral by the department of psychiatry)
As the psychiatrist evaluated and we got to know that pt was abstinent from 1 month so they have ruled out the psychological cause.
But as the pts attenders have told us that after his wife’s death he started behaving differently.
On the second day of admission as the fever spikes were still high we planned for a lumbar puncture to rule out any meningeal infection (pt also had neck stiffness)
After the lumbar puncture results we came to a conclusion that patient has BACTERIAL MENINGITIS. Patient was started on antibiotics.
2) Why was the patient intubated?
Ans: He was intubated in view of hypoxia.
Firstly patient was on ACMV-VC mode of ventilation
On the second day as he was able to breath on its own the mode was changed to SIMV-VC mode.
On day 6 of admission pt was removed from the ventilator and put on t-piece as the saturations were fair and ABG was improved.
3) Did the bacterial infection resolve?
Ans: For the same we performed a second lumbar puncture and sent the csf for evaluation and we got to know that infection has been subsided.
But the patient still had fever spikes and even developed a bed sore at the sacral region.
4) Why there were still fever spikes and delirium ?
Ans: We suspected may be the patient has got any infection because of ventilator (VAP) or can be sepsis due to the bed sore.
So we sent samples for culture
Blood
Urine
Et tube cultures (were sent when the pt was still intubated)
C/S swab from the bed sore.
After the results we got to know that
In urine: e.coli growth was detected (for which medication was started)
5) What did we do for bed sore?
Ans: For bed sore we consulted the General Surgery department for which they said
>Alternate day dressings
>frequent change of position
>Mobility of the patient
For the dressing respective unit Surgery PG used to come and for the rest our icu sisters, interns and pt attenders have done the needful.
6) Why was the patient still delirious?
Ans: For which we again consulted our Psychiatry department and they started patient on
Tab.Olanzapine 2.5mg
7) Procedures done:
>assisted in intubating the patient
>did ambu to pt
>have put foleys catheter and ryles tube to the pt
>assisted in 2 lumbar puncture procedures
>assisted in dressing of the bed sore
>have taken blood samples and ABG of the pt
8) But unfortunately pt LEFT AGAINST MEDICAL ADVICE due to personal reasons.
We tried to be in contact with the attenders but they were not having access to technology so we couldn’t connect with them on online platforms. And when we tried calling them but they did not respond.
Case 5:
1) Why were pts extremities cold and clammy?
Ans: As the pt extremities are cold and clammy and had low blood pressure so we could suggest of CARDIOGENIC SHOCK and possibly can be HEART FAILURE
(Confirmation by ECG and other investigations)
2) What type of MI did pt have ?
Ans: Pt had suffered with Non ST elevated MI we can confirm it by our ECG
Factors favouring in our pt:
Age,
Body fat (f/m ratio we calculated=3.88),
Can be due to dietary intake of excess sodium and even fatty foods
3) Why was the pt intubated?
Ans: when pt presented to us she was already in hypoxic state (64%) and her ABG readings were also suggesting hypoxia so we planned for intubation. Firstly pt was placed on ACMV-VC mode of mechanical ventilator.
4) What was the further plan of treatment ?
Ans: As patient suffered from a MI we started pt on inotropic support and other systemic medication.
Pt was having active movement of left limbs but decreased movements of the right side.
5) What could be the reason for decreased right side movements?
Ans: For the further we planned for a CT-Brain, but as the pt was not in a condition to shift to ct the plan was delayed and first preference was given for stability of the pt and her heart.
After pt became stable we planned for CT-Brain and we found out that pt has a large left side brain lesion covering almost of parietal and temporal region.
As we could observe pt was only able to have active movement of the left side and right side hemiparesis was present. Pt had spontaneous eye opening but the eyes were deviated on the side of the lesion.
6) What could we do for the lesion?
Ans: We immediately started the pt on anti platelets and even took a neurologist referral for the same. Our neurologist also suggested the same medication.
7) Why was the pt febrile?
Ans: When the pt came to us she was afebrile but from the 5th day of admission we could see fever spikes. We had sent samples for cultures and even started symptomatic treatment.
Culture reports were normal and fever was subsiding with symptomatic treatment. Further evaluation we got to know that pt has developed a bed sore on her right buttock. That could be the reason of her fever spikes.
8) What was the further plan?
Ans: As our pt was responding really well and ABG readings were also fair suggestive of extubation. Pt was extubated on day 12th and then was maintained on O2. Inotropic support was also stopped as the cardiogenic shock was resolved. As on regular investigations on chest xray we found to have right side lung haziness and clinically decreased air entry was present on that side, so for further evaluation we asked for x-ray reporting from our Radiology department. On conclusion we found out that our pt had right side lung lower lobe collapsed and some findings suggested of VAP(this also could be the reason for our fever spikes)
9) We started treatment for the same and pt was responding on it but the fever spikes were still present.On day 19 we planned to send for cultures again and even central line cultures were sent. On day 20 pt need for O2 decreased and she was responding well. But by evening she started gasping and again O2 was raised. We sent for an ABG and by that we founded that pt was in hypoxic state and by 7pm her health started detoriating. We planned for re-intubating the pt and started the process but unfortunately pt saturations started to fall down rapidly and we initiated CPR (according to AHA 2020 rules:
https://cpr.heart.org/-/media/cpr-files/cpr-guidelines-files/highlights/hghlghts_2020_ecc_guidelines_english.pdf) After 30 mins of CPR also the pt did not respond and was declared dead.
10) Procedures done:
>assisted in intubating the patient
>did central line sutures to pt
>have put foleys catheter and ryles tube to the pt
>assisted in taking pt for ct brain with the help of bain circuit
>assisted in dressing of the bed sore
>have taken blood samples and ABG of the pt
>performed CPR on the pt
>did Physiotherapy of chest and all four limbs of the pt
Case 6:
1) What could be the reason of her seizure? Can it be post-partum eclampsia?
Ans: As the pt was presented 10 days post-partum so we suspected of post-partum eclampsia for the same OBG department was called. They gave us a conclusion that if she would have seizures within 4-5 days after delivery then it could be called post-partum eclampsia but as it is already 10 days post delivery so it cannot be due to post partum eclampsia.
But according to the litreture study post partum eclampsia can be upto 4 wks after delivery
2) What is the primary treatment u must give to a pt presenting with seizures?
Ans: If pt presented with the episode or after an episode firstly we must give Lorazepam 2cc and put a mouth gag to prevent tongue bite. After stabilising the pt we must start them on anti epileptics (levipill 1gm in 100ml NS) to prevent further episodes of seizures.
3) What is the plan?
Ans: We took the pt for an Emergency MRI as she had 2 episodes of seizures even after giving primary treatment.
But the MRI showed normal findings and other organic causes were also ruled out.
Further we planned for an EEG
4) What were the other symptoms present?
Ans: pt also complained of severe headache (frontal) and was not subsiding on medication and rest, it was also associated with fever spikes.
We prescribed a PCM 650mg fever got subsided but headache was still present. We were not able to give heavy medications as she was breastfeeding the neonate.
5) But unfortunately pt LEFT AGAINST MEDICAL ADVICE for their personal reasons.
We tried being in touch with the pt and attenders, they were in contact with us for 3 days n we got the information that she did not have any other episode of seizure but the headache was persistent. After that he stopped contacting us and when we tried to contact they did not respond.
Case 7:
Case 8:
27/9-01/10
WARD DUTY:
- Helped my co interns by making SOAP notes.
- Conducted classes for junior batches in the morning and for PGs in the afternoon session and recorded videos of the classes.
- Monitored patients in the ward as guided by concerned unit PG and helped them by updating the ward patients.
- Updating about the newly admitted cases in ICU,AMC and as well as WARD.
- Helped our long distance patients by taking them to referrals and even helped for blood transfusion during surgery.
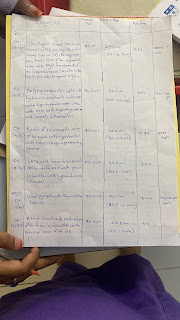
Helped our 1st year PG by doing thesis work by measuring FM ratio by me and my co intern(Raveena). We were guided by our 3rd yr PG Sir.
Procedure:
For mid arm circumference we measured from acromian process to olecrenon process and took the midway measurement between the two bony points And then measured the skin fold thickness with our callipers and then subtracted the mid arm circumference with the callipers value to get our muscle mass.For Visceral fat we took umbilicus as our reference and measured it’s girth After getting both values we divided visceral fat with Mac(mac-skinfold thickness) to get our ratio.
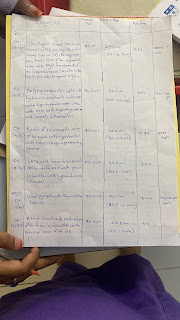

28/m
79 - visceral fat
26.5 -0.4 26.1- MAC- FAT
3.02-FM ratio
Diagnosis: Liver abscess , No comorbidities
100.5-visceral fat
35- 0.8- MAC- FAT
2.93- FM ratio
Diagnosis: Foot drop.
02/10-06/10
NEPHRO DUTY:
Handled Day care patients who came for dialysis.
Learnt about central line and fistula for dialysis.
Handled cases which came in emergencies with help of my PGs.
Learnt about dialysis machine and what all infections a pt can get by not maintaining proper hygiene of the central line
Learnt about drugs used in hypo and hypertension.
Made an elog of our pt
Case 9:
07/10-11/10
ICU & AMC DUTY:
Monitored vitals of all pts hourly
Maintenance of ventilator settings as guided by the respective PG.
Taken ABGs and have taken samples for lab investigations.
Learnt how to manage in critical situations.
Learnt stabilisation of pt in critical situations.
ADDITIONALS:
Have assisted in 4 intubations.
Have put 4 ryles tube and 3 foleys catheter.
Have taken ABG samples and other samples
Have done ascitic tap to a pt
Have done CPR to 2 pts
Have done Ambu for 4 pts
Have presented in class and discussed about my cases with the faculty and HOD sir
Have convinced one of our pt attenders to not LEAVE AGAINST MEDICAL ADVICE and give us chance to treat the pt
Have assisted in Dressings of bed sores and ulcer
Thankful to our respected HOD, SRs, PGs and my fellow interns for guiding me and helping me in all the possible ways.
Special mentions:
Dr.Rakesh Biswas (HOD)
Dr.Vinay
Dr.Raveen
Dr.Manasa
Dr.Saicharan
Dr.Venkat Sai
Dr.Pavani
Dr.Deepika
Dr.Bharath
Dr.Nishitha
My co-interns
Dr.Harsha
Dr.Meghna
Dr.Raveena


Comments
Post a Comment