MEDICAL CASE
This is an E log book to discuss our patient's de-identified health data shared after taking his guardian's signed informed consent. Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable comments in comment box are most welcomed
I have been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my cmpetancy i reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
December 14 2021
YOGITA AILANI
Roll no:149
CASE DISCUSSION
23 YEARS OLD PATIENT PRESENTED WITH INVOLUNTARY MOVEMENTS OF BOTH UPPER LIMBS AND LOWER LIMBS
HISTORY OF PRESENTING ILLNESS
Sequence of events in patient’s life that might have led to the present condition:-
AT BIRTH:
She was born in the month of September 1998
Non Consanguineous marriage
First born child, full term baby
Normal Vaginal delivery
Cried immediately at birth
Weight of the baby at birth 2.5kg
Was admitted to the hospital for 3 Days as she engulfed amniotic fluid (3ltrs of fluid aspirated from the mouth)
Prelactal feeds were given for 3 days
Baby was given to mother on the 3rd day and she started breastfeeding
Child was breastfed (along with supplemental feeds) for 6 months of life and then stopped.
AT 1 YEAR OF AGE:
Abnormal movements were observed of both UL & LL which were rapid and jerky lasted for 1 min
Episodes were observed in both day and night time
Mostly after getting up from bed
No H/o vomitings, loss of consciousness
H/o frequent fever, throat pain, cough, cold present
H/o delayed milestones
H/o behavioural changes - anger, anxiety, crying spells
AT 3 YEARS OF AGE: (2001)
Started on Valproate and regular follow up monthly
In the month of April
C/o Inability to walk since 15 to 20 days
Associated with Fever
O/E:
Deep Tendon Reflexes- Absent
Plantar_ B/L Flexors??
Rx- Syp. Potklor
In the month of May
CT - Normal
EEG - Abnormal Stage II sleep recorded and Interictal discharges bihemispherically.
AT 7 YEARS OF AGE: (2005)
Stopped AED??
Patient continued to have these episodes during sleep, more during early mornings, preceeded by brief arousal from sleep.
H/o Episodes + while getting up from sleep, standing after prolonged sitting, stress, during erection
(Few times during cycling)
Patient was aware of this episodes, followed by her leg pains used to stop activity before it starts.
AT 13 YEARS OF AGE:(2011)
EEG- Normal
Rx-
TAB. Tetrabenazine 25mg 1/2 Tab at Night.
TAB. Valproate 300mg BD
TAB. Clonazepam 0.5mg OD
AT 16 YEARS OF AGE: (2014)
Vitamin D- 4.21 (< 10 deficient)
Started on Vit. D capsule
( 1 TAB a week for 6 months)
- MRI (normal)
Patient continued to have similar episodes
H/o injuries to both limbs due to hitting the surroundings during the episodes
AT 19 YEARS OF AGE:(2017)
Started Ayurveda medicines along with Tetrabenazine and clonazepam for 5-6 months.
AT 20 YEARS OF AGE:(2018)
Started on Oxcarbazepine
(150- x -300mg)
- Video EEG done- Episodes in Favour of Paroxysomal Hypnogogic Choreoathetosis
Stopped medication for 2 years.
AT 23 YEARS OF AGE: (2021)
Since past 2 months patient is having increased frequency of these episodes, more during the night, even on slight movement during sleep(3-4 hrs), lasting less than a minute along with pain in lower limb joints.
-H/o anger bursts at family members, decreased activity, depressed mood since 2 months.
- skin lesions over buttocks and both limbs since 2 months
- patient has Throat Pain since 2 months
- difficulty in swallowing
-Since 1month she developed increased involuntary movements of whole body
Involuntary movements are present mostly during sleep last for 1-5min
Sometimes she develop involuntary movements when she stands up from prolonged sitting position.
PAST HISTORY
Not a k/c/o DM, HTN, epilepsy, asthma.
patient has H/o heat and Cold intolerance
patient has H/o recurrent oral ulcers
PERSONAL HISTORY
Diet : Mixed
Appetite : normal
Sleep : normal
Bowel and bladder : normal
Addictions : none
FAMILY HISTORY
Paternal grandfather had h/o seizures in his childhood
GENERAL EXAMINATION
The patient was conscious, coherent and co operative.
She was well Oriented to time, place and person.
Icterus - Absent
Pallor - Absent
Clubbing - Absent
Cynosis - Absent
Lymphadenopathy - Absent
Edema - Absent
VITALS (on the day of admission)
temperature : afebrile
pulse rate : 84bpm
respiratiory rate : 14cpm
blood pressure : 120/80mmHg
spo2 at room air : 98% at RA
SYSTEMIC EXAMINATION
- CVS: S1.S2 HEARD
- RS: BAE+, NVBS +
- P/A: SOFT, NON TENDER
- CNS Examination : NAD
INVESTIGATIONS
- Other opinions were taken from respective departments for some secondary issues the patient has
- ENT opinion in v/o throat pain and pain during swallowing
- DVL opinion in v/o itchy lesions over gluten region and both lower limbs
- Psychiatry referral - adjustment disorder due to physical illness
PROVISIONAL DIAGNOSIS
Chorea?
Acute pharyngitis
Ulcers
Eczema
PEDIGREE CHART
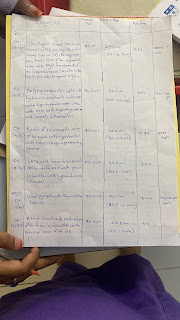
Day wise progress of PATIENT
Day 1
S-c/o throat pain
1 fever spike yesterday
O- pt had 16 episodes of choreiform movements yesterday night ,each lasting less than a minute
Pt - conscious, coherent
Afebrile
Pr 100 /min
Bp 120/70 mmhg
Rr cpm
Spo2 98 % on room air
Cvs- s1s2+
Rs- b/l air entry +
Ophthalmology referral taken - no KF rings
Dvl opinion in v/o itchy lesions over gluten region and both lower limbs
Ent opinion in v/o throat pain and pain during swallowing- mild congestion in posterior pharyngitis wall and anterior pillars
Psychiatry referral - adjustment disorder due to physical illness
?dissociative motor disorder
A- ? Benign hereditary chorea
Acute pharyngitis
Ulcers secondary to ? Folliculitis, trauma with
Eczema
Adjustment disorder
P- To start on tab tetrabenazine 12.5 mg po bd
Tab Augmentin 625mg po bd
Tab levocitrezine 10mg po od
Salt water gargles
Momate f cream for local application bd
Mupirocin gel for local application bd
Day 2
S- c/o Disturbed sleep
throat pain decreased
No fever spikes
O- pt had 14 episodes of choreiform movements yesterday night ,each lasting less than a minute
Pt - conscious, coherent
Afebrile
Pr 86 /min
Bp 120/70 mmhg
Rr 16cpm
Spo2 98 % on room air
Cvs- s1s2+
Rs- b/l air entry +
Ophthalmology referral taken - no KF rings
Dvl opinion in v/o itchy lesions over gluten region and both lower limbs
Ent opinion in v/o throat pain and pain during swallowing- mild congestion in posterior pharyngitis wall and anterior pillars
Psychiatry referral - adjustment disorder due to physical illness
?dissociative motor disorder
A- ? Benign hereditary chorea
Acute pharyngitis
Ulcers secondary to ? Folliculitis, trauma with
Eczema
Adjustment disorder
P-
Tab Augmentin 625mg po bd
Tab levocitrezine 10mg po od
Salt water gargles
Momate f cream for local application bd
Mupirocin gel for local application bd
Day 3
S- c/o Disturbed sleep
throat pain decreased
No fever spikes
O- pt had 25 episodes of choreiform movements yesterday night ,each lasting less than a minute
Pt - conscious, coherent
Afebrile
Pr 84 /min
Bp 120/70 mmhg
Rr 16cpm
Spo2 98 % on room air
Cvs- s1s2+
Rs- b/l air entry +
Ophthalmology referral taken - no KF rings
Dvl opinion in v/o itchy lesions over gluten region and both lower limbs
Ent opinion in v/o throat pain and pain during swallowing- mild congestion in posterior pharyngitis wall and anterior pillars
Psychiatry referral - adjustment disorder due to physical illness
?dissociative motor disorder
A- ? Benign hereditary chorea
Acute pharyngitis
Ulcers secondary to ? Folliculitis, trauma with
Eczema
Adjustment disorder
P-
Tab Augmentin 625mg po bd
Tab levocitrezine 10mg po od
Salt water gargles
Momate f cream for local application bd
Mupirocin gel for local application bd
To collect sample for 24hr urinary copper from today mrng.
Day 4
S- c/o Disturbed sleep
throat pain decreased
No fever spikes
O- pt had 28episodes of choreiform movements yesterday night ,each lasting less than a minute. Frequency and intensity of episode has increased
Pt - conscious, coherent
Afebrile
Pr 84 /min
Bp 120/70 mmhg
Rr 16cpm
Spo2 98 % on room air
Cvs- s1s2+
Rs- b/l air entry +
Ophthalmology referral taken - no KF rings
Dvl opinion in v/o itchy lesions over gluten region and both lower limbs
Ent opinion in v/o throat pain and pain during swallowing- mild congestion in posterior pharyngitis wall and anterior pillars
Psychiatry referral - adjustment disorder due to physical illness
?dissociative motor disorder
A- ? Benign hereditary chorea
Acute pharyngitis
Ulcers secondary to ? Folliculitis, trauma with
Eczema
Adjustment disorder
Iron deficiency anemia sec to ? Nutritional
P-
Tab Augmentin 625mg po bd
Tab levocitrezine 10mg po od
Salt water gargles
Momate f cream for local application bd
Mupirocin gel for local application bd
To send samples for serum copper , cerruloplasmin and 24hr urinary copper excretion today and discharge her




















Comments
Post a Comment