MEDICAL CASE
This is an E log book to discuss our patient's de-identified health data shared after taking his guardian's signed informed consent. Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable comments in comment box are most welcomed
I have been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my cmpetancy i reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
January 27 2022
YOGITA AILANI
Roll no:149
75year old male presented to GM OPD with chief complaints of
- Cough with expectoration since 1 month
- Shortness of Breath since 1 month, aggravating since 7 days
- Pedal edema since 7 days
HISTORY OF PRESENTING ILLNESS:-
Patient was apparently asymptomatic 2 years ago ,later he developed SOB,pedal edema and generalised weakness for 2 weeks and for which he was treated.
2 months ago he developed cough with sputum , which is white in color, not blood stained and non foul smelling. And also SOB which gradually progressed from Grade 3 to Grade 4 ,one month ago.
He also developed facial puffiness 20 days back . Along with pedal edema with is of pitting type.He has chest pain since 10 days which aggrevated with SOB.
No H/O fever with rash,hemoptysis,nausea,vomiting,constipation.
PAST HISTORY:-
Not a k/c/o HTN,DM,Thyroid,asthma,epilepsy,Congenital heart Disease.
PERSONAL HISTORY:-
Diet-mixed
Appetite-normal
Bowel and bladder movements-Regular
Sleep -adequate
Addictions-chronic smoker since 30 yrs (4 chutas per day)
Occasionally alcohol (stopped 2 yrs back)
GENERAL EXAMINATION:-
Patient is conscious , coherent and cooperative and well oriented to time place
and person,
Thin built and moderately nourished
Pallor- present
Bilateral Pedal Edema-present
Icterus- absent
Cyanosis- absent
Clubbing- absent
Lymphadenopathy- absent
Weight loss of 4kgs within 1 day after diuretics.
VITALS:-
Temperature- 98.6 F
Pulse rate- 92 bpm(Irregularly regular)
Respiratory rate-14cpm
BP- 110/80 mm Hg
Spo2- 112%
GRBS-130 mg%
SYSTEMIC EXAMINATION:-
Respiratory system.
Inspection-
Shape of chest-elliptical and symmetrical
Position of trachea-midline.
Bilateral symmetrical chest movements on respiration.
Palpation-
No local rise of temperature and no tenderness.
Apexbeat
TVF
Percussion-
Ascultation-
crepts heard over right infra mammary and infra axillary regions.
CVS- S1 S2 +,No murmurs
P/A- soft, non tender
CNS- No FND.
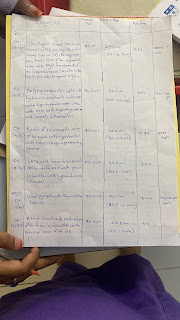
INVESTIGATIONS:-
ECG
Chest Xray

Hemogram:-
Hb- 6.2
Microcytic hypochromic with anisopoikilocytosis
RBC-3million
Platelets-2 lakhs
Electrolytes:-
Na+2 -145
K+ - 4.2
Cl- -100
ESR-40
Provisional diagnosis:
Acute on Chronic COPD with Right Heart Failure and with Rt lower lobe pneumonia.
TREATMENT:-
Inj lasix 40 mg /IV/BD ( if SBP>110/80)
Inj Augmentin 1g/IV/BD
Tab Azithromycin 500mg PO/OD.
Inj optineuron 1 amp in 100ml NS/ IV/OD.
Inj thiamine 1 amp in 100ml NS/IV/BD.
Nebulisation with Duolin, budecort,mixomist-1 respule 6th hourly.
Tab tamiflu 75mg po/bd.
Tab pan 40 mg po/od
Fluids restriction (<1.5L/day) and salt restriction (<4g/day).
Daily weight monitoring.










Comments
Post a Comment