48 YEARS OLD FEMALE WITH MULTISYSTEM INVOLVEMENT
MEDICAL CASE
This is an E log book to discuss our patient's de-identified health data shared after taking his guardian's signed informed consent. Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable comments in comment box are most welcomed
I have been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency i reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
March 29, 2022
YOGITA AILANI
Roll no:149
- Shortness of breath since 1 month
- Difficulty in swallowing since 1 month
- Pedal edema since 1 week
- Chest tightness since 1 week.
- HYPERTENSION 8years back- taking regular medication
- HYPOTHYROIDISM 6years back- taking regular medication
- Rheumatoid arthritis 6 years back(no proper reports were shown presently and no medication is been taken)
- DM type-2 5 months back- not on medication
- MILIARY TB 1 month back- started on ATT (stopped)
Pulse rate : 78 beats/min
BP : 140/90 mm Hg
RR : 18 cpm
SpO2 : 98% at room air
GRBS : 105mg/dl
- Alopecia - Present
- Eyes - Proptosis seen, no conjunctival suffusion
- EOM - Intact
- Bald, red tongue seen
- No ulcers
- No thyroid swelling
- Skin - Multiple hyper pigmented macules seen all over face, upper limbs, neck, thigh, abdomen and upper back.
- Dry skin present ; Thickening of skin over forearms, dorsum of hand and fingers and on and around mouth.
- Hair is absent over the macules.
- Slight peeling is still present over the arms and legs.
- RESPIRATORY EXAMINATION:
INSPECTION: Movements of chest appears to be decreased on the left side in comparison to right side.
PALPATION: Vocal fremitus decreased in left mamary , ISA area in comparison to other areas.
PERCUSSION: Dull note in left mamary area and ISA area.
AUSCULTATION: Decreased air entry on left ISA,IMA area. Right side - normal air entry. Bilateral vesicular breathing noted. Tubular breathing heard on right inter-scapular area.
coarse crepitations - end inspiratory - no variation with cough - heard on left ISA >>right ISA.
- CVS EXAMINATION:
S1,S2 heard
No murmurs. No palpable heart sounds. - PER ABDOMEN:
Soft, Non-tender
No organomegaly
Bowel sounds heard
no guarding/rigidity - CNS EXAMINATION:
No focal neurological deficits
Gait- NORMAL
RBS: 70mg/dl
HbA1c : 6.8%
RFT:
Blood Urea: 136mg/dl
S. Creatinine: 4.8mg/dl
Na 139
K 3.0
Cl 102
HEMOGRAM:
HB 7.2
TC 15,000
MCV 80.4
PCV 21.5
MCH 27.0
MCHC 33.6
PLT 3.67
RDW 62
Peripheral smear - NORMOCYTIC, NORMOCHROMIC
Serum iron : 45ug/dl
ABG:
pH 7.34
PCo2 18.8
PaO2 92.4
HCO3 12.2
SpO2 96
LFT:
TB 2.8
DB 0.74
AST 14
ALT 10
ALP 673
TP 7.4
ALB 2.23
CUE:
ALB ++
Sugars nil
Pus cells plenty
Epithelial cells 1-2
COVID-19 RAT - NEGATIVE
ESR - 180
CRP - POSITIVE (1.2 mg/dl)
RA FACTOR - NEGATIVE .
LDH - 326 IU/L
- Few small volume mediastinal lymph nodes noted
- Both lungs are studded with tiny nodular densities - miliary TB or ILD?
- Small air filled cyst noted left lower lobe.
- No evidence of effusion.
- Non-obstructive left renal calculus.
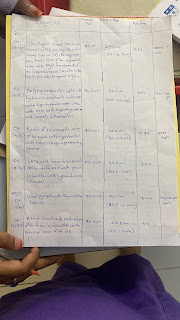
- Tab. Rifampicin 600mg PO OD
- Tab. Isoniazid 300mg PO OD
- Tab. Ethambutol 900mg PO OD
- Neb. Budecort BD
- Tab. Pulmoclear PO BD
- Tab. Amlong 5mg PO OD
- Tab. Thyronorm 50mcg PO OD
- Tab. Benadon 40mg PO OD
- Protein powder 1scoop + glass milk PO BD
- Liquid paraffin all over the body
- Mucopain gel
- Inj. HUMAN ACTRAPID (only when glucose levels are high)

.jpeg)