MEDICAL CASE
This is an E log book to discuss our patient's de-identified health data shared after taking his guardian's signed informed consent. Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable comments in comment box are most welcomed
I have been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency i reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
March 06, 2022
YOGITA AILANI
Roll no:149
CASE DISCUSSION
50 year male Farmer by occupation came with chief complaints of
- Fever since 10 days,
- Lethargy since 4 days ,
- Blood in saliva since 3 days and
- SOB since 2 days
HISTORY OF PRESENTING ILLNESS
Patient was apparently alright 10 days back then he had low grade fever , intermittent , relieved on taking medication . Not associated with chills and rigors and was able to perform his routine works. From 4 days as patient was lethargic and taken to local hospital found out to be Dengue NS 1 + and platelet count was
44,000 on day 1
22,000 on 2nd day
Following one SDP transfusion, it became
33,000 on 3rd day
From 3 days patient notices blood in saliva during coughing and Black coloured stools from 2 days , patients SOB progressed from Grade 2 --- Grade 4 ( MMRC ).
PAST HISTORY
Not known case of Diabetes, Hypertension , Asthma , TB , Epilepsy .
CLINICAL IMAGES
PERSONAL HISTORY
DIET: mixed
APPETITE: Normal
SLEEP: adequate
BOWEL AND BLADDER: regular
ADDICTIONS: Alcohol intake daily 30ml whiskey
FAMILY HISTORY
Not significant
GENERAL EXAMINATION
Patient is examined in a well lit room with adequate exposure, after taking the consent of the patient.
he is conscious, coherent and cooperative, moderately built and nourished.
no signs of pallor, edema, icterus, cyanosis, clubbing, lymphadenopathy
VITALS
Temperature : Afebrile
Pulse rate : 78 beats/min
BP : 140/90 mm Hg
RR : 18 cpm
SpO2 : 98% at room air
GRBS : 105mg/dl
SYSTEMIC EXAMINATION
- RESPIRATORY EXAMINATION: Bilateral air entry present, ronchi are heard
- CVS EXAMINATION:
S1,S2 heard
No murmurs. No palpable heart sounds.
- PER ABDOMEN:
Soft, Non-tender
No organomegaly
Bowel sounds heard
no guarding/rigidity
- CNS EXAMINATION:
No focal neurological deficits
Gait- NORMAL
PROVISIONAL DIAGNOSIS
SEVERE ARDS with Dengue NS 1 reactive with Thrombocytopenia .
( H/O 1 SDP and 1 FFP transfusion )
INVESTIGATIONS
HEMOGRAM:
HB 9.8
TC 12600
MCV 81.7
PCV 31.8
MCH 27.0
MCHC 33.6
PLT 17000
ABG:
pH 7.4
PCo2 27.4
PaO2 59.7
HCO3 19.5
SpO2 91










TREATMENT
1. IVF NS , RL @ 75 ml/hr
2. Daily postural BP monitoring
3. W/F Bleeding manifestation
4. I/O strict monitoring
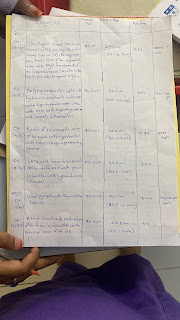
S.O.A.P notes
5/3/22
S :
Fever and SOB
O :
PATIENT IS CONCIOUS , COHERENT COOPERATIVE
NO PALOR, ICTRUS, CLUBBING , CYANOSIS , LYMPHADENOPATHY , EDEMA
VITALS -
TEMPERATURE - 98.1
PULSE RATE - 60 bpm
BLOOD PRESSURE - 110/70 MM OF HG
RESPIRATORY RATE -
SPO2 - 100 % AT 4 lit O2
I - 1900 ml
O - 500 ml
SYSTEMIC EXAMINATION -
PER ABDOMEN : NON DISTENDED, SOFT NON-TENDER, NO GAURDING/RIGIDITY
CARDIOVASCULAR SYSTEM : S1 AND S2 HEARD , NO MURMURS
RESPIRATORY SYSTEM : BILATERAL AIR ENTRY PRESENT, RONCHI HEARD
CENTRAL NERVOUS SYSTEM : NAD
A :
ARDS with Dengue NS 1 reactive with Thrombocytopenia . ( H/O 1 SDP and 1 FFP transfusion )
P :
1. IVF NS , RL @ 50 ml/hr
2. W/F Bleeding manifestation
3. Strict I/O charting
4. BP monitoring
6/3/22
S :
Fever and SOB
O :
PATIENT IS CONCIOUS , COHERENT COOPERATIVE
NO PALOR, ICTRUS, CLUBBING , CYANOSIS , LYMPHADENOPATHY , EDEMA
VITALS -
TEMPERATURE - 98.1
PULSE RATE - 60 bpm
BLOOD PRESSURE - 110/70 MM HG
RESPIRATORY RATE - 35 cpm
SPO2 - 100 % AT 4 lit O2
I - 2000 ml
O - 1050 ml
HB - 10.8 4/3/22
10.1 5/3/22
9.8 6/3/22
Pt - 17000 4/3/22
18000 5/3/22
52000 6/3/22
SYSTEMIC EXAMINATION -
PER ABDOMEN : NON DISTENDED, SOFT NON-TENDER, NO GAURDING/RIGIDITY
CARDIOVASCULAR SYSTEM : S1 AND S2 HEARD , NO MURMURS
RESPIRATORY SYSTEM :
B/LAE+,inspiratory crepts present in (RT>LT) infraaxillry , infrascapular areas
CENTRAL NERVOUS SYSTEM : NAD
7/3/22
S :
Fever ( subsided ) and SOB
O :
PATIENT IS CONCIOUS , COHERENT COOPERATIVE
NO PALOR, ICTRUS, CLUBBING , CYANOSIS , LYMPHADENOPATHY , EDEMA
VITALS -
TEMPERATURE - 98.4
PULSE RATE - 60 bpm
BLOOD PRESSURE - 120/70 MM HG
RESPIRATORY RATE - 20 cpm
SPO2 - 98 % AT 2 lit O2
HB - 10.8 4/3/22
10.1 5/3/22
9.8 6/3/22
10.1 7/3/22
Pt - 17000 4/3/22
18000 5/3/22
52000 6/3/22
50000 7/3/22
SYSTEMIC EXAMINATION -
PER ABDOMEN : NON DISTENDED, SOFT NON-TENDER, NO GAURDING/RIGIDITY
CARDIOVASCULAR SYSTEM : S1 AND S2 HEARD , NO MURMURS
RESPIRATORY SYSTEM :
B/LAE+,inspiratory crept’s present in (RT>LT) infraaxillry , infrascapular areas
CENTRAL NERVOUS SYSTEM : NAD
A :
Dengue NS 1 reactive , IgM positive with Thrombocytopenia, with Mild ARDS
P:
1. IVF NS , RL @ 50 ml/hr
2. W/F Bleeding manifestation
3. Strict I/O charting
4. BP monitoring















Comments
Post a Comment