MEDICAL CASE
This is an E log book to discuss our patient's de-identified health data shared after taking his guardian's signed informed consent. Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable comments in comment box are most welcomed
I have been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my cmpetancy i reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
March 8, 2022
YOGITA AILANI
Roll no:149
A 50 year old male patient construction worker by occupation came with complaints of
- Loss of appetite since 25 days
- pain in bilateral loin region since 25 days
HISTORY OF PRESENTING ILLNESS:-
Patient was apparently asymptommatic 2 years back when he went to the hospital with complaints of loss of appetite and was diagnosed to have renal failure and hypertension.
Patient was advised for dialysis from 2019 and was having dialysis in other hospital till 2020.
Then in 2021 he came to our hospital and had 2-3 dailysis after which dialysis was stopped and he was on conservative management and had regular follow ups.
He came with complaints of loss of appetite since 25 days and pain in bilateral loin region since 25 days
No history of decreased urine output, pedal edema, shortness of breath, chest pain, palpatations, cough.
History of usage of NSAID's (3-4/day) because of bilateral knee joint pains, pricking type which was aggravated with work and relieved by taking medication.
PAST HISTORY:-
He was diagnosed with hypertension 2 yrs back
Was advised medication Tab. Amlong 2.5mg and Tab. Arkamin100mg
Not a k/c/o of DM,thyroid disorders,BA,TB,epilepsy
Appetite: loss of appetite
Diet:Mixed
Sleep: Adequate
Bowel habits: regular
Bladder habits:regular
No addictions
FAMILY HISTORY:-
No similar complaints in the family
GENERAL EXAMINATION:-
Patient is conscious , coherent and cooperative and well oriented to time place
and person,
Moderately built and moderately nourished
Pallor- present
Icterus- Absent
Cyanosis- Absent
Clubbing- Absent
Lymphadenopathy- Absent
Edema: Absent
CLINICAL IMAGES:-
VITALS:-
BP-140/90 mm hg
PR- 86 bpm
Temp- afebrile
RR- 20 cpm
Spo2- 98% on room air
SYSTEMIC EXAMINATION:-
CVS: S1 S2 +, no murmurs
RS: BAE+, NVBS,no added sounds
CNS: NAD
P/A: distended, soft, non tender, BS+
PROVISIONAL DIAGNOSIS:-
CHRONIC KIDNEY DISEASE SECONDARY TO ? NSAID'S ABUSE
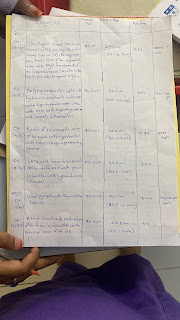
INVESTIGATIONS:-
CXR:-
USG:
ABG:
ph:7.20
po2:49.0mmhg
pco2:21.0mmhg
hco3:7.9mmol/l
LFT:
TB:0.60mg/dl
DB:0.16mg/dl
SGOT:16IU/L
SGPT:15IU/L
PROTEINS:7.5gm/dl
ALBUMIN:3.6gm/dl
A/G RATIO:0.92
RFT:
UREA:185mg/dl
CREATININE:12.8mg/dl
URIC ACID:7.7mg/dl
HEMOGRAM:
Hb:6.5gm/dl
WBC:9800cells/cumm
SMEAR:normocytic,normochromic,Anemia
BLOOD GROUP: A+ve
CUE:
COLOUR: PALE YELLOW
APPEARANCE: clear
PUS CELLS: 4-5 cells/HPF
RBC: NILL
TREATMENT:-
1.Fluid restirction <1.5 l/ day
2. Salt restriction <2-4 g/ day
3. TAB. LASIX 40 MG PO BD
4. TAB NODOSIS 500MG PO BD
5. TAB SHELCAL CT PO OD
6. TAB. OROFER XT PO OD
7. INJ SODIUM BICARBONATE 100 MEQ






Comments
Post a Comment