LONG CASE: FINAL PRACTICAL
MEDICAL CASE
This is an E log book to discuss our patient's de-identified health data shared after taking his guardian's signed informed consent. Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable comments in comment box are most welcomed
I have been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency i reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
June 6, 2022
YOGITA AILANI
Hall ticket No:1701006002
CASE DISCUSSION:
A 40 years old Male, resident of bhongir, painter by occupation presented to OPD with chief complaints of
- Shortness of breath since 7 days
- Chest Pain on left side since 5days
Patient was apparently asymptomatic 7days back then developed shortness of breath which was
- insidious in onset
- gradually progressive (grade I to grade II according to MMRC)
- Chest pain:
non radiating
nature: pricking type - loss of weight(about 10kgs in past 1yr)
- loss of appetite
- Vomitings
- Orthopnea, PND
- Edema
- palpitations
- Wheeze
- chest tightness
- cough
- hemoptysis
- Diabetes Mellitus 3 yrs back (on medication- Metformin 500mg, Glimiperide 1mg)
- Mixed diet
- sleep is adequate ( but disturbed from past few days)
- loss of appetite is present
- bowel and bladder movements are regular
- He used to Consume
Alcohol stopped 20years back ( 90ml per day)
Smoking from past 20years (10 cigarettes per day) but stopped 2years back.
Pulse rate : 139beats/min
BP : 110/70 mm Hg
RR : 45 cpm
SpO2 : 91% at room air
GRBS : 201mg/dl
- RESPIRATORY EXAMINATION:
INSPECTION:
Shape of chest is elliptical,
B/L asymmetrical chest,
Trachea in central position,
Expansion of chest- Right- normal, left-decreased,
Use of Accessory muscles is present.
PALPATION:
All inspectory findings are confirmed,
No tenderness, No local rise of temperature,
trachea is deviated to the right,
Measurement:
AP: 24cm
Transverse:28cm
Right hemithorax:42cm
left hemithorax:40cm
Circumferential:82cm
Tactile vocal fremitus: decreased on left side ISA, InfraSA, AA, IAA.
PERCUSSION: Stony dull note present in left side ISA, InfraSA, AA, IAA.
AUSCULTATION:
B/L air entry present, vesicular breath sounds heard,
Decreased intensity of breath sounds in left SSA,IAA,
Absent breath sounds in left ISA.
- CVS EXAMINATION:
S1,S2 heard
No murmurs. No palpable heart sounds.
JVP: normal
Apex beat: normal - PER ABDOMEN:
Soft, Non-tender
No organomegaly
Bowel sounds heard
no guarding/rigidity - CNS EXAMINATION:
No focal neurological deficits
Gait- NORMAL
Reflexes: normal
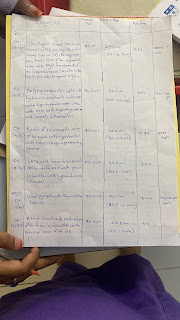
DB: 0.74mg/dl
AST: 24IU/L
ALT: 09IU/L
ALP: 167IU/L
TP: 7.5gm/dl
ALB: 3.29gm/dl
INTERPRETATION: As 2 values are greater than the normal we consider as an EXUDATIVE EFFUSION.
(confirmation after pleural fluid c/s analysis)
- O2 inhalation with nasal prongs with 2-4 lt/min to maintain SPO2 >94%
- Inj. Augmentin 1.2gm/iv/TID
- Inj. Pan 40mg/iv/OD
- Tab. Pcm 650mg/iv/OD
- Syp. Ascoril-2tsp/TID
- DM medication taken regularly
- High Protein diet
- 2 egg whites/day
- Monitor vitals
- GRBS every 6th hourly









Comments
Post a Comment