SHORT CASE: FINAL PRACTICAL
MEDICAL CASE
This is an E log book to discuss our patient's de-identified health data shared after taking his guardian's signed informed consent. Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable comments in comment box are most welcomed
I have been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency i reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
June 6, 2022
YOGITA AILANI
Hall ticket no:1701006002
CASE PRESENTATION:
A 45 year old lady, resident of Nalgonda, Tailor by occupation presented to GM OPD with chief complaints of
- Fever since 3months
- Body pains since 3months
- loss of appetite since 3months
- Appearance of facial rash since 10days
Patient had a history of diminution of vision which started at the age of 15 years.
For which she was advised use of
- To use spectacles
- Optic atrophy with macular degeneration in both the eyes.
Not a known case of DM/HTN/ASTHMA/CAD /EPILEPSY/TB
PERSONAL HISTORY:
Diet- mixed
Appetite- decreased
Bowel and bladder- regular
Sleep- disturbed
Addictions- nil
FAMILY HISTORY:
No similar complaints in the family.
GENERAL EXAMINATION :
Pallor present
no signs of edema, icterus, clubbing, cyanosis, lymphadenopathy.
VITALS:
Pulse rate : 72beats/min
BP : 110/70 mm Hg
RR : 18 cpm
SpO2 : 98% at room air
SYSTEMIC EXAMINATION:
CVS:
INSPECTION: shows no scars on the chest, no features of raised JVP, no additional visible pulsations seen.
PALPATION: all inspectory findings are confirmed, apex beat normal at 5th ics medial to mcl, no additional palpable pulsations or murmurs
PERCUSSION: showed normal heart borders
AUSCULTATION:S1 S2 heard no murmurs or additional sounds
CNS:
C/C/C
MOTOR-: normal tone and power
reflexes: RT LT
BICEPS ++ ++
TRICEPS ++ ++
SUPINATOR ++ ++
KNEE ++ ++
SENSORY : touch, pressure, vibration, and proprioception are normal in all limbs.
GIT:
INSPECTION: normal scaphoid abdomen with no pulsations and scars
PALPATION: all inspectory findings are confirmed, no organomegaly, non tender and soft PERCUSSION: normal resonant note present, liver border normal
AUSCULTATION: normal abdominal sounds heard, no bruit present.
RESPIRATORY:
INSPECTION: normal chest shape bilaterally symmetrical, mediastinum central
no scars, Rr normal, no pulsations
PALPATION: Insp findings are confirmed
PERCUSSION: normal resonant note present bilaterally
AUSCULTATION: B/L air entry present, vesicular breath sounds heard.
PROVISIONAL DIAGNOSIS:
? Secondary sjogren syndrome
Anemia
B/L Optic atrophy
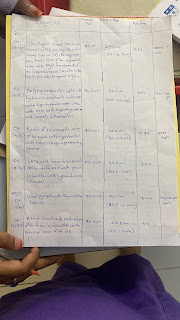
INVESTIGATIONS:
RBS: 136mg/dl
HEMOGRAM:
HB: 6.9
TC: 9700
MCV: 85.1
PCV: 21.7
MCH: 27.1
MCHC: 31.8
PLT: 1.57
ESR: 90
SMEAR: ANISOCYTOSIS
RFT:
Blood Urea: 20mg/dl
S. Creatinine: 1.1mg/dl
Na: 136
K: 3.3
Cl: 98
LFT:
TB: 0.45
DB: 0.17
AST: 60
ALT: 17
ALP: 138
TP: 6.3
ALB: 2.18
CUE:
ALB +
Sugars nil
Pus cells nil
ESR - 90
CRP - NEGETIVE
HCV: NEGETIVE
HBV: NEGETIVE
HIV: NEGETIVE
TREATMENT:
- Tab. Pan 40mg/PO/OD
- Tab. Deflazocort 6mg/PO/BD
- Tab. cefixime 200mg/PO/BD
- Tab. Orofex-XT (15 mins before food)/PO/OD
- Tab. Teczine 10mg/PO/OD
- Hydrocortisone cream 1%/LA/OD for 1 week (on face).
- GRBS every 6th hourly
- Monitor vitals.





.jpeg)


Comments
Post a Comment