This is an E log book to discuss our patient's de-identified health data shared after taking his guardian's signed informed consent. Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable comments in comment box are most welcomed
I have been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency i reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CASE DISCUSSION:
A 75 year old male came with complaints of
- fever since 10 days
- altered sensorium since 5 days
HOPI:
Patient was apparently asymptomatic 10 days back and then developed fever which was high grade not associated with chills and rigor. Then he developed altered sensorium since 5 days he was not able to recognise his family members.
PAST HISTORY:
Not a K/C/O DM, HTN, TB,EPILEPSY, ASTHMA
Has hypo-pigmented patches on b/l lower limbs and b/l nipples since 6 years using herbal medication regularly, itching is present.
PERSONAL HISTORY:
He is Married
He consumes
- Mixed diet
- sleep is adequate
- Appetite normal
- bowel and bladder movements are regular
- He Consumes Alcohol twice a week (90ml) since 50 years presently abstinent since 15 days
- He smokes beedi 1-2 packs/day since 55 years
FAMILY HISTORY: no similar complaints in the family.
DAILY ROUTINE: Wakes up early in the morning around 5:00am and then goes to the farm, comes back home at 10:00am has breakfast (Tea and bread or some tiffin), from 10:00am to 6:00pm he stays home takes rest and does house chores. Takes his meals on time (3 meals/day).
Sleeps at 10:00pm and the routine continues.
CLINICAL IMAGES:
GENERAL EXAMINATION:
Patient is conscious ,non-cooperative, not oriented to time, place and person.
Thinly built and nourished.
VITALS:
BP: 120/70mmhg
PR: 90bpm
RR: 20cpm
Temp: 100f
SYSTEMIC EXAMINATION:
RS:
Inspection : barrel shape
Decreased breath sounds on right side
Diffuse expiratory wheeze
CVS: s1,s2 no added sounds
P/A: not tender
Pt is altered
GCS - E3V1M6
Speech - making incomprensible sounds
Pupils:NSRL
Motor
Power : Not moving his left upper limb and lower limb as actively as right side
Tone : Normal
Reflexes : B T S A K P
R: - - - - - Flexion
L : - - - - - Flexion
Neck rigidity : Present
Kerning's : Positive
Brudzski : Negative
PROVISIONAL DIAGNOSIS: ALTERED SENSORIUM UNDER EVALUATION
INVESTIGATIONS:
On Day1
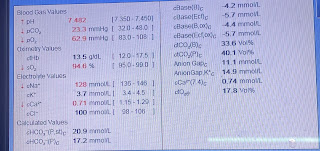
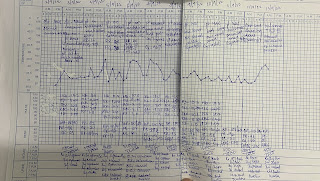
ABG: Day 1 at 10:43pm
ABG: Day 1 at 11:51pm
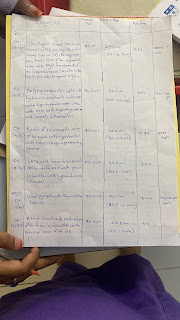
LP PROCEDURE 1:
2D ECHO:
TREATMENT:
1.INJ.CEFTRIAXONE 2gm IV/STAT then 1gm IV/BD
2.INJ.IVF DNS 50ml/hr
3.INJ.PANTOP 40mg IV/OD
4.INJ.ZOFER 4mg IV/SOS
5.INJ.OPTINEURON 1AMP IN 100ml NS IV/OD
6.MONITOR VITALS EVERY 6th hrly
7.GRBS MONITORING EVERY 4th
Day 2
S: fever since 10 days and altered sensorium since 5 days
Presently altered sensorium
O: pt is conscious,uncooperative,not oriented to time,place and person.
BP: 120/70mmhg
PR: 90bpm
RR: 20cpm
Temp: 98.6f
SYSTEMIC EXAMINATION:
RS:
Inspection : barrel shape
Decreased breath sounds on right side
Diffuse expiratory wheeze
CVS: s1,s2 no added sounds
P/A: not tender
CNS:
Pt is altered
GCS - E3V1M6
Speech - making incomprensible sounds
Motor
Power : Not moving his left upper limb and lower limb as actively as right side
Tone : Normal
Reflexes : B T S A K P
R: - - - - - Flexion
L : - - - - - Flexion
Neck rigidity : Present
Kerning's : Positive
Brudzski : Negative
A: ?Altered sensorium under evaluation
?Alcohol withdrawal syndrome
P:
1.INJ.CEFTRIAXONE 2gm IV/STAT then 1gm IV/BD
2.INJ.IVF DNS 50ml/hr
3.INJ.PANTOP 40mg IV/OD
4.INJ.ZOFER 4mg IV/SOS
5.INJ.OPTINEURON 1AMP IN 100ml NS IV/OD
6.MONITOR VITALS EVERY 6th hrly
7.GRBS MONITORING EVERY 4th hrly
INVESTIGATIONS:
ABG: Day 2 at 6:17 am
ABG: Day 2 at 4:46pm
Plan: Patient intubated on ACMV VC MODE as he was hypoxic Post Intubation Ventilator Settings :
RR - 16
Fio2 - 40
PEEP - 5
TV - 400
Post Intubation Vitals :
Pupils - B/L Fixed Pin point Pupils
BP - 100/70mmHg
PR - 116/Min
RR - 22/Min
Spo2 - 100%
Midaz Infusio - 5ml/hr
Atracurium Infusion - 10ml/hr
ABG:Day 2 at 9:50pm
Day 3
S:pt is on mechanical ventilator and sedation
O: pt on SIMV VC mode
RR TOTAL: 29
RR:20
Fio2:30%
PEEP: 5 cm of H2O
TV:400
VITALS:
BP: 110/70mmhg
PR: 82bpm
RR: 16cpm
Temp: 98.5f
SYSTEMIC EXAMINATION:
CVS: s1,s2 no added sounds
P/A: not tender
A: Altered sensorium secondary to meningitis with type 1 respiratory failure with acute exacerbation of COPD.
P:
TREATMENT:
1.INJ.CEFTRIAXONE 2gm IV/STAT then 1gm IV/BD
2.RT FEEDS 100ml milk 4th hrly, 50ml water 2nd hourly
3.INJ.PANTOP 40mg IV/OD
4.INJ.ZOFER 4mg IV/SOS
5.INJ.OPTINEURON 1AMP IN 100ml NS IV/OD
6.Inj.NEOMOL IV if TEMP>102f sos
7.GRBS MONITORING EVERY 4th hrly
8.Inj.MIDAZ 5ml/hr
9.Tab. Azithromycin 500mg PO/OD
CT SCAN BRAIN:
Day 3 At 9:30 am
Pt was able to breath on its own so the changes were done to SIMV -VC Mode
RR Total - 29
RR - 16
Fio2 - 30
PEEP - 5
VT - 400
Vitals -
BP - 100/80
RR - 38/min
HR - 108/min
Spo2 - 97
ABG: Day 3 at 12:20pm
ABG: Day 3 at 9:20pm
On Day 4
S:pt is on mechanical ventilator and sedation
O: pt on SIMV VC mode
RR TOTAL: 29
RR:20
Fio2:30%
PEEP: 5 cm of H2O
TV:400
VITALS:
BP: 110/70mmhg
PR: 97bpm
RR: 16cpm
Temp: 97.6f
SYSTEMIC EXAMINATION:
CVS: s1,s2 no added sounds
P/A: not tender
A: Altered sensorium secondary to meningitis with type 1 respiratory failure with acute exacerbation of COPD.
P:
TREATMENT:
1.INJ.CEFTRIAXONE 2gm IV/STAT then 1gm IV/BD
2.RT FEEDS 100ml milk 4th hrly, 50ml water 2nd hourly
3.INJ.PANTOP 40mg IV/OD
4.INJ.ZOFER 4mg IV/SOS
5.INJ.OPTINEURON 1AMP IN 100ml NS IV/OD
6.Inj.NEOMOL IV if TEMP>102f sos
7.GRBS MONITORING EVERY 4th hrly
ABG: Day 4 At 9:00am
ABG: Day 4 at 10:36pm
ABG: Day 5 at 6:30am
Day 5
S:pt is on mechanical ventilator and sedation
O: pt on SIMV VC mode
RR TOTAL: 34
RR:16
Fio2:21%
PEEP: 5 cm of H2O
TV:400
VITALS:
BP: 130/70mmhg
PR: 122bpm
RR: 20cpm
Temp: 100.8f
SpO2: 97%
GRBS: 327 mg/dl
SYSTEMIC EXAMINATION:
CVS: s1,s2 no added sounds
P/A: not tender
CNS:
Doll’s eye reflex +
Pt is unresponsive
GCS - E1VTM1
Pupils:B/L equal constricted and reacting to light.
R L
Corneal + +
Conjunctival. +. +
Tone : Hypotonia
Reflexes : B T S A K P
R: - - - - - Flexion
L : - + - - - Flexion
A: Altered sensorium secondary to meningitis with type 1 respiratory failure with acute exacerbation of COPD.
P:
TREATMENT:
1.INJ.CEFTRIAXONE 2gm IV/STAT then 1gm IV/BD
2.RT FEEDS 100ml milk 4th hrly, 50ml water 2nd hourly
3.INJ.PANTOP 40mg IV/OD
4.INJ.ZOFER 4mg IV/SOS
5.INJ.Dexamethasone 4mg BD
6.Inj.NEOMOL IV if TEMP>102f sos
7.GRBS MONITORING EVERY 4th hrly
8.INJ.Clexane 40mg S/C OD
9.Tab. Azithromycin 500mg PO/OD
10.NEB BUDECORT 12th hrly DUOLINE 8th hourly
11.Monitor vitals
Day 5 at 3:50pm
Day 6
S:pt removed from ventilation and was put on T. Piece since today morning 7.30 am
O:
Pt conscious
GCS:E4VTM4
spontaneous eye opening +
Spontaneous breathing +
VITALS:
BP: 120/70mmhg
PR: 137bpm
RR: 30cpm
Temp: 101.3f
SpO2: 98%
GRBS: 197 mg/dl at 8:00am
SYSTEMIC EXAMINATION:
CVS: s1,s2 no added sounds
P/A: not tender,Soft
A: fever with Altered sensorium secondary to meningitis with type 1 respiratory failure with acute exacerbation of COPD.
P:
Plan to extubate
ABG: Day 6 at 6:20am
ABG: Day 6 at 9:30am
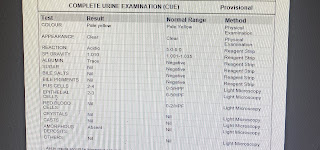
Urine culture report:
Day 7
S:pt extubated yesterday at 4:00pm
Bed sores at sacral area
O:
Pt conscious
GCS: E4V5M3
spontaneous eye opening +
Spontaneous breathing +
VITALS:
BP: 120/70mmhg
PR: 98bpm
RR: 33cpm
Temp: 98.7f
SpO2: 98%
GRBS: 335 mg/dl at 8:00am
CSF reports awaiting
URINE CULTURE:
isolated E.coli sensitive to :
Nitrofurantoin
Gentamicin
Cotrimoxazole
Fosfomycin
Amikacin
Tazobactum
Clavulenic acid
Meropenam
SYSTEMIC EXAMINATION:
CVS: s1,s2 no added sounds
P/A: not tender,Soft
RS:BAE+
A: fever with Altered sensorium secondary to meningitis with type 1 respiratory failure with acute exacerbation of COPD, BED SORES + (sacral area Grade II)
P:
RT FEEDS 100ml milk 4th hrly, 50ml water 2nd hrly
Inj.PAN 40mg/IV/OD
Inj.Zofer 4mg/IV/SOS
Inj.Neomol 1gm/IV/TEMP>102f
Neb with budecort 12th hrly, duoline 8th hourly
Frequent change of position every 2nd hrly
Procedures: LP Procedure done at 8:00am today
ABG:Day 7 at 6:00pm








Day 8
S:
Bed sores at sacral area
O:
Pt conscious
GCS: E4V5M3
spontaneous eye opening +
Spontaneous breathing +
VITALS:
BP: 120/70mmhg
PR: 92bpm
RR: 22cpm
Temp: 98.5f
GRBS: 345mg/dl at 8:00am
SYSTEMIC EXAMINATION:
CVS: s1,s2 no added sounds
P/A: not tender,Soft
RS:BAE+
A: fever with Altered sensorium secondary to meningitis with type 1 respiratory failure with acute exacerbation of COPD, BED SORES + (sacral area Grade II)
P:
RT FEEDS 100ml milk 4th hrly, 50ml water 2nd hrly
Inj.PAN 40mg/IV/OD
Inj.Zofer 4mg/IV/SOS
Inj.Neomol 1gm/IV/TEMP>102f
Neb with budecort 12th hrly, duoline 8th hourly
Frequent change of position every 2nd hrly
ABG: day 8 at 6:00am



Day 9
S:
Bed sores at sacral area
O:
Pt conscious
GCS: E4V5M3
spontaneous eye opening +
Spontaneous breathing +
VITALS:
BP: 120/70mmhg
PR: 92bpm
RR: 22cpm
Temp: 98.5f
GRBS: 345mg/dl at 8:00am
SYSTEMIC EXAMINATION:
CVS: s1,s2 no added sounds
P/A: not tender,Soft
RS:BAE+
A: fever with Altered sensorium secondary to meningitis with type 1 respiratory failure with acute exacerbation of COPD, BED SORES + (sacral area Grade II)
P:
RT FEEDS 100ml milk 4th hrly, 50ml water 2nd hrly
Inj.PAN 40mg/IV/OD
Inj.Zofer 4mg/IV/SOS
Inj.Neomol 1gm/IV/TEMP>102f
Neb with budecort 12th hrly, duoline 8th hourly
Frequent change of position every 2nd hrly
ABG: day 9 at 8:00am



Day 10
S:
Bed sores at sacral area
Dressing is done
O:
Pt conscious
GCS:E4V4M3
VITALS:
BP: 110/70mmhg
PR: 96bpm
RR: 30cpm
Temp: 98.5f
GRBS: 195mg/dl at 8:00am
SYSTEMIC EXAMINATION:
CVS: s1,s2 no added sounds
P/A: not tender,Soft
RS:BAE+
A: fever with Altered sensorium secondary to meningitis with type 1 respiratory failure with acute exacerbation of COPD, BED SORES + (sacral area Grade II)
P:
Mobilise him with support
RT FEEDS 100ml milk 4th hrly, 50ml water 2nd hrly
Inj.PAN 40mg/IV/OD
Inj.Zofer 4mg/IV/SOS
Inj.Neomol 1gm/IV/TEMP>102f
Neb with budecort 12th hrly, duoline 8th hourly
Frequent change of position every 2nd hrly
Day 11
S:
Bed sores at sacral area grade 2-3
O:
Pt conscious
GCS:E4M6V3
VITALS:
BP: 110/70mmhg
PR: 94bpm
RR: 26cpm
Temp: 98F
GRBS: 235mg/dl at 8:00am
SYSTEMIC EXAMINATION:
CVS: s1,s2 no added sounds
P/A: not tender,Soft
RS:BAE+
A: fever with Altered sensorium secondary to meningitis with type 1 respiratory failure with acute exacerbation of COPD, BED SORES + (sacral area Grade II)
P:
Mobilise him with support
RT FEEDS 100ml milk 4th hrly, 50ml water 2nd hrly
Inj.PAN 40mg/IV/OD
Inj.Zofer 4mg/IV/SOS
Inj.Neomol 1gm/IV/TEMP>102f
Neb with budecort 12th hrly, duoline 8th hourly
Frequent change of position every 2nd hrly
Day 12
S:
Bed sores at sacral area grade 2-3
Irrelevant talk
O:
Pt conscious, not oriented to time,person
GCS:E4M6V3
VITALS:
BP: 110/70mmhg
PR: 82bpm
RR: 26cpm
Temp: 98.6f
GRBS: 124 mg/dl at 8:00am
SYSTEMIC EXAMINATION:
CVS: s1,s2 no added sounds
P/A: not tender,Soft
RS:BAE+
A: fever with Altered sensorium secondary to meningitis with type 1 respiratory failure with acute exacerbation of COPD, BED SORES + (sacral area Grade II)
P:
Mobilise him with support
Inj.PAN 40mg/IV/OD
Inj.Zofer 4mg/IV/SOS
Inj.Neomol 1gm/IV/TEMP>102f
Neb with budecort 12th hrly, duoline 8th hourly
Frequent change of position every 2nd hrly with ambulation.



















































































Comments
Post a Comment