55 YEAR OLD MALE WITH C/O FEVER AND SOB
This is an E log book to discuss our patient's de-identified health data shared after taking his guardian's signed informed consent. Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable comments in comment box are most welcomed
I have been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CASE DISCUSSION:
A 55 year old male came with chief complaint of
- FEVER SINCE 3 days
- SOB SINCE MORNING
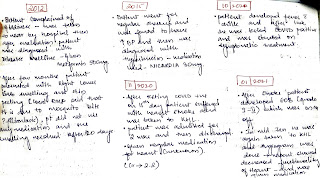
PAST HISTORY:
k/c/o DM since 10yrs on medication GLIZED 80 (sulfonylurea)
k/c/o HTN since 7yrs on medication NICARDIA 30mg
K/c/o CKD ON MHD since 3 months
Last session of dialysis on 1/10/22
PERSONAL HISTORY:
He is a contractor by occupation
Consumes mixed diet
Appetite normal
Bowel n bladder regular
Sleep adequate
Addictions: Used to consume alcohol since 30 years- occasionally but stopped 6yrs back due to family pressure
FAMILY HISTORY:
No similar complaints in family
CLINICAL IMAGES:
GENERAL EXAMINATION:
Pt is conscious, coherent and cooperative
Moderately built and nourished.
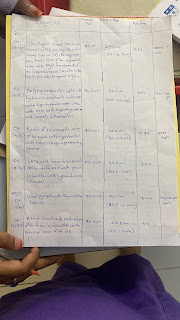
On admission:
BP:140/80mmhg
PR:146bpm
RR:24cpm
SPO2: 90% on RA
GRBS: 163mg/dl
SYSTEMIC EXAMINATION:
CVS: S1,S2, +
RS: BAE+
P/A: soft, non tender
CNS: NAD
PROVISIONAL DIAGNOSIS:
SOB UNDER EVALUATION
K/c/o CKD ON MHD since 3 months














Comments
Post a Comment